Imaging is an essential part of managing many serious fungal infections, especially in deep tissues such as the lungs or CNS
At the moment this page focuses on Aspergillus but feel free to contact us if you would like to contribute information about other yeasts and moulds
Diagnosis
Characteristic signs (e.g. reverse halo, signet ring, HAM)
Severity and extent of invasion
Staging of chronic conditions
Monitoring
Inactive fungal nodules or aspergillomas may be monitored to determine when (or even whether) to start antifungal treatment
Response to antifungal treatment may be seen on CT scans (e.g. cavity walls may become thinner upon successful treatment)
Treatment
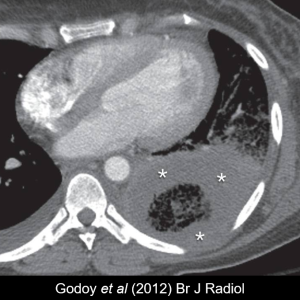
Bronchial artery embolization may be required to manage life-threatening haemoptysis in CPA patients in whom the artery has become eroded
Radiology of aspergillosis
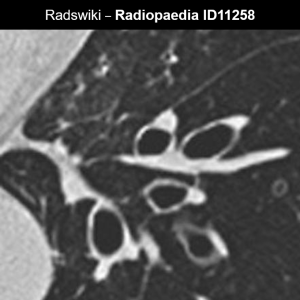
Slugs
Rabbit ears
HAM
Signet ring
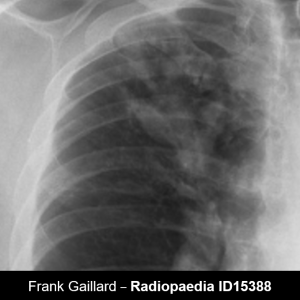
ABPA
Allergic bronchopulmonary aspergillosis (ABPA) is a hypersensitivity condition seen in patients with asthma or CF, where the immune system reacts excessively against Aspergillus mould growing in the lungs
Early in the course of disease, radiological signs are often transient and many radiographs appear normal. Infiltrates and consolidation appear during exacerbations as sticky mucus plugs block airways, then disappear when are coughed up
Over time, irreversible dilatation of the airways may occur. Central bronchiectasis is more typical of ABPA, but it is not uncommon for it to extend to the periphery. Varicose and cystic forms are more typical
Occasionally aspergillomas may develop. End-stage patients may show fibrosis and spontaneous pneumothorax
ABPA in asthma: ISHAM diagnostic guidelines (Agarwal et al, 2013) includes “Radiological features consistent with ABPA” as one of the minor criteria
ABPA in CF: Radiological signs of these conditions are largely overlapping. The Cystic Fibrosis Foundation consensus criteria (Stevens et al, 2003) reviews the evidence for each sign in more detail
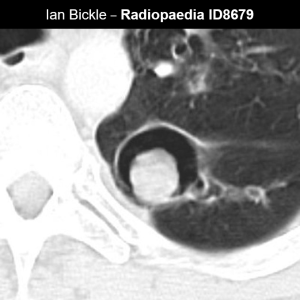
Aspergilloma
Monod sign
Cavity wall thickness
Bronchial artery erosion
Subacute invasive aspergillosis (SAIA)
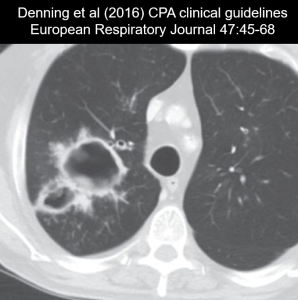
CPA
Chronic pulmonary aspergillosis (CPA) is a long-term infection where Aspergillus grows saprophytically inside a cavity or other site of structural damage
ITS radiological appearance is highly variable so CT scans are preferable to plain radiographs. Note that patients who have previously lived in a resource-limited setting may have only received X-rays
It is particularly seen in the upper lobes and is more commonly single (but may be multiple or bilateral). It often forms in cavities caused by TB or lung cancer, or alongside conditions such as NTM, bronchiectasis, sarcoidosis or ABPA. It is particularly common in COPD patients whose lung immunity against Aspergillus spores is weakened
If CPA is inadequately treated, it can eventually lead to extensive fibrosis
Imaging is a crucial component of CPA diagnosis despite ITS variable appearance. ERS diagnostic criteria for CPA (Denning et al, 2016) specify that thoracic imaging must be consistent with CPA, preferably based on CT scan
Halo sign
Reverse halo
Air crescent
IPA
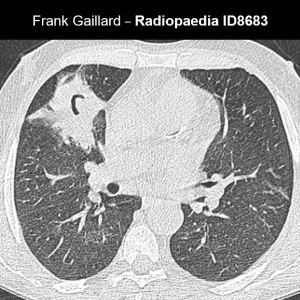
Invasive pulmonary aspergillosis (IPA) is a life-threatening acute infection seen mainly in immunocompromised (especially neutropaenic) patients, particularly in critical care and haemato-oncology settings.
ITS radiological appearance evolves over the course of the infection and typical signs are not seen in all patients, particularly in children (Burgos et al 2008)
Parenchymal lesions
Extra-axial lesions
Complications
Abscess vs neoplasm
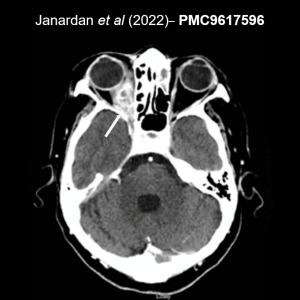
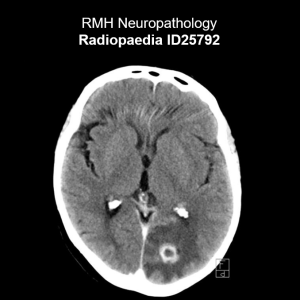
CNS abscess
In rare cases, Aspergillus can disseminate to the brain from an initial infection site in the lungs or sinuses, or following previous brain pathology (Janardan et al, 2022). This is mainly seen in immunocompromised patients and causes a range of nonspecific neurological symptoms such as headache, lethargy, seizures, and altered mental status
Radiological appearance is often not distinct from other conditions such as neoplasms or bacterial infections, so a definitive diagnosis generally requires mycological evidence (microscopic identification of fungal elements or culture) from needle aspiration or open biopsy. CSF culture is